Clark melanocytic nevi (CMN) are a special type of acquired, circumscribed, pigmented lesions that represent disordered proliferations of variably atypical melanocytes. CMN arise de novo or as part of a compound melanocytic nevus. CMN are clinically distinctive from common acquired nevi: larger and more variegated in color, asymmetric in outline, irregular borders; they also have characteristic histologic features. CMN are regarded as potential precursors of superficial spreading melanoma and also as markers of persons at risk for developing primary malignant melanoma of the skin, within the dysplastic nevus or on “normal” skin.
Causes of the Clark Melanocytic Nevus
Multiple loci, including 1p36 and 9p21, have been implicated in familial melanoma/dysplastic nevus syndrome. The abnormal clone of melanocytes can be activated by exposure to sunlight. Immunosuppressed patients (renal transplantation) with dysplastic nevi have a higher incidence of melanoma. Dysplastic nevi favor the exposed areas of the skin, and this is related to the degree of sun exposure. Dysplastic nevi may, however, occur on the covered areas (e.g., hairy scalp or groin).
Symptoms of the Clark Melanocytic Nevus
Atypical nevi can occur anywhere on the body, and usually begin to appear at puberty. They may however, be more common in sun-exposed areas, the back, and the legs.
Diagnosis
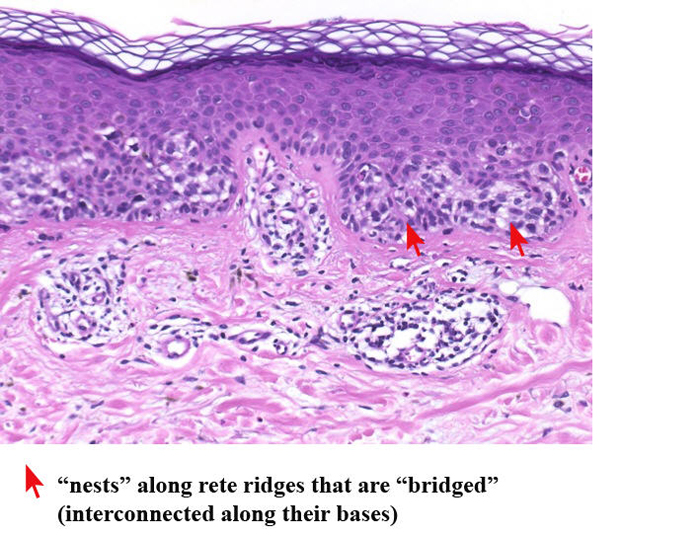
The diagnosis of CMN is made by clinical recognition of typical distinctive lesions, and diagnostic accuracy is considerably improved by epiluminescence microscopy; one of these lesions should be excised for histologic confirmation of the diagnosis of CMN. The clinicopathologic correlations are now well documented. Siblings, children, and parents also should be examined for CMN once the diagnosis is established in a family member.
Anatomic association (in contiguity) of dysplastic nevi has been observed in 36% of sporadic primary melanomas, in about 70% of familial primary melanomas, and in 94% of melanomas with familial melanoma and dysplastic nevi.
Treatment
Surgical excision of lesions with minimal margins. Laser or other types of physical destruction should never be used because they do not permit histopathologic verification of diagnosis. The following guidelines for selection of lesions to be excised are suggested:
- Lesions that are changing (increase in size, change in pigmentation pattern, changes in shape and/or border).
- Lesions that cannot be closely followed by the patient by self-examination (on the scalp, genitalia, upper back).
Patients with dysplastic nevi in the familial melanoma setting need to be followed carefully: in familial dysplastic nevi, every 3 months; in sporadic dysplastic nevi, every 6 months to one year. Search for changes in existing dysplastic nevi and development of new nevi. Photographic follow-up is important with Polaroid prints of the trunk and extremities; also Polaroid prints (1:1) of larger lesions (>6 mm) and all lesions that have some variegation. Patients should be given color-illustrated pamphlets that depict the clinical appearance of CMN, malignant melanoma, and common acquired nevomelanocytic nevi. Patients with dysplastic nevi (familial and nonfamilial) should not sunbathe and should use sunscreens when outdoors. They should not use tanning parlors. Family members of the patient should also be examined regularly.
References
- https://www.ncbi.nlm.nih.gov/pubmed/10188841
- https://www.humanpathol.com/article/S0046-8177(99)90191-0/pdf
- https://emedicine.medscape.com/article/1058445-overview