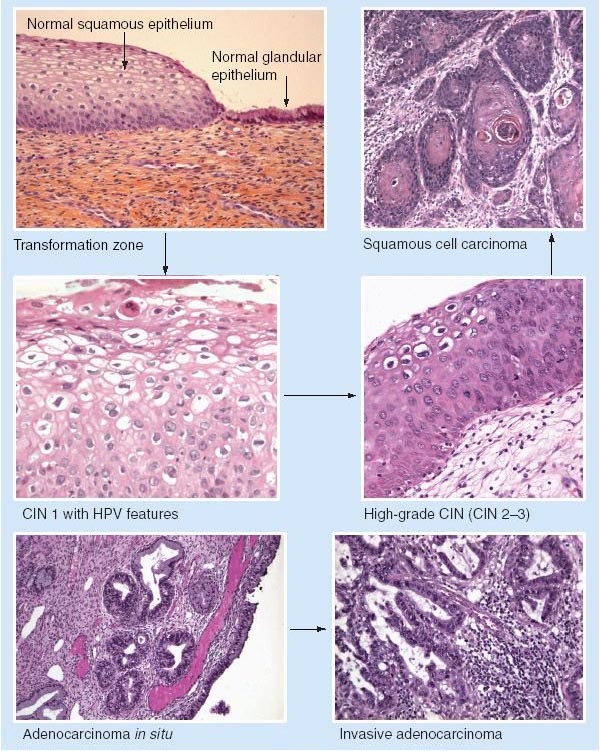
Human papillomavirus (HPV) infection of the anogenital epithelium can result in a spectrum of changes referred to as squamous intraepithelial lesions (SILs), ranging from mild dysplasia to squamous cell carcinoma (SCC) in situ (SCCIS). Over time, these lesions can regress, persist, progress, or recur, in some cases to invasive SCC. Clinically, lesions appear as multifocal macules, papules, plaques on the external anogenital region. Lesions involving the cervix and anus have the highest risk for transformation to invasive SCC; however, lesions can transform at any site.
Causes
HPV-16 and -18 infected cells may not be able to differentiate fully as a result of either (a) functional interference of cell cycle-regulating proteins, caused by viral gene expression (e.g., interaction between HPV-16 E6 with cellular protein p53, interaction between HPV-16 E7 with cellular protein pRB) or (b) over-production of E5, E6, and E7. When this occurs, the host DNA synthesis continues unchecked and leads to rapidly dividing undifferentiated cells with morphologic characteristics of intraepithelial neoplasias. Accumulated chromosomal breakages, rearrangements, deletions, and other genomic mutations in these cells lead to cells with invasion capability and, ultimately, to cervical malignancy.
Symptoms
In situ SCC presents as one or more flat red scaly patches up to several centimetres wide, often found in large numbers on the lower legs. These patches are also known as ‘Bowen’s disease’. ‘In situ’ means the malignant cells are confined to the epidermis, the outside layer of the skin. In situ SCC can persist as such or develop into invasive SCC
Diagnosis
Clinical suspicion, confirmed by biopsy of lesion.
Treatment
Colposcopy
A colposcope is a binocular microscope used to examine the cervix, providing magnification (6- to 40-fold) and illumination. The most common indication for colposcopy is abnormal exfoliative cytology. Acetic acid, 3 to 5%, is applied to the cervix, which causes columnar and abnormal epithelium to become edematous. Abnormal (atypical) epithelium adopts a white or opaque appearance that can be distinguished from the normal pink epithelium. Abnormal epithelium is then biopsied. Colposcopy can also be performed on individuals with abnormal anal exfoliative cytology, and biopsy specimens obtained from abnormal site(s).
Biopsy of Lesions In cases of documented SIL or SCCIS, biopsy specimens should be obtained from rapidly enlarging lesions, areas of ulceration or bleeding, exuberant tissue with abnormal vascularity.
Local Therapy of SIL The only way of possibly reducing the potential risk of invasive SCC with its morbidity and mortality is diagnosis and eradication of intraepithelial disease. In that lesions are relatively uncommon, cases are often best managed by a dermatologist with clinical experience in the care of these patients, an oncologic gynecologist, or a colorectal surgeon. If lesion biopsy specimens do not show early invasion, lesions can be treated medically or surgically.
Medical Management 5-fluorouracil cream has been used but is difficult to use because of erosions. Imiquimod cream 5% is also effective.
Surgical Management Surgical excision, Mohs’ surgery, electrosurgery, laser vaporization, cryosurgery.
References